Development and characterisation of artificial materials for ocular surface reconstruction
Contact
Director of the Department of Ophthalmology
Head of the Laboratory for Experimental Ophthalmology
Office at Pius-Hospital Oldenburg
Address
Development and characterisation of artificial materials for ocular surface reconstruction
The human cornea is part of the anterior segment of the eye and is essential for vision. It is around 500 µm thick and essentially consists of three cellular layers: the outer epithelium, the stroma and the inner endothelium, which are separated from each other by two thin acellular layers, Bowman's lamella and Descemet's membrane. The stroma makes up around 90 per cent of the corneal thickness and itself consists of 75 per cent water, three to ten per cent keratocytes and extracellular matrix. This extracellular matrix is secreted by the keratocytes and consists mainly of collagen and proteoglycans.
Diseases of the ocular surface, such as neurotrophic keratopathy, ocular pemphigoid, Stevens-Johnson syndrome, infections or burns/chemical burns can lead to corneal erosions, the formation of corneal ulcers, substance defects and scarring. This can be accompanied by an impairment of the transparency and surface curvature of the cornea, leading to a reduction in vision or even complete loss of vision.
Worldwide, pathological changes to the cornea are the third most common cause of blindness after cataracts and glaucoma. There are no drug therapy options for most permanent corneal dysfunctions, so that often only surgical measures can preserve or restore the patient's vision. Amniotic membrane (the innermost membrane of the amniotic sac; AM for short) is usually used to heal persistent or progressive corneal epithelial defects. This can be used as a transferable cover for mechanical protection of the regenerating corneal epithelium (onlay) or as a transplant that is inserted into the corneal defect and acts as a basement membrane substitute (inlay). AM has a favourable cell growth-stimulating, anti-inflammatory and anti-angiogenic effect. However, the disadvantages include the poor standardisability of the tissue, the risk of infection transmission from donor to recipient and the significantly limited transparency, which restricts visual function postoperatively. In addition, the low biomechanical strength of the tissue often leads to loss of the transplant.
For the treatment of stromal corneal defects, a transplantation of human donor corneal tissue in the form of a lamellar or penetrating keratoplasty is performed in order to restore vision. In addition to the risk of graft rejection, the main limiting factor here is the limited availability of suitable donor material. For this reason, alternatives to amniotic membrane transplantation as well as to the transplantation of human donor corneas are currently the subject of these research projects. Two different approaches are being pursued: on the one hand, the use of the body's own cells, which are stimulated to synthesise a matrix and are therefore highly biocompatible for patients, and on the other hand, matrices made from biomaterials, which can be produced in a standardised and GMP-compliant manner.
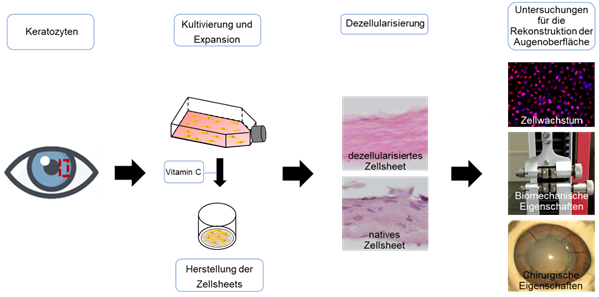
In vitro cultured human corneal stromal replacement for ocular surface reconstruction
A promising approach for the reconstruction of the corneal stroma is the stimulation of human corneal keratocytes to secrete extracellular matrix. The advantage of such in vitro-generated replacement tissue is that it can be produced from the recipient's own cell material, thus eliminating rejection reactions against the donor tissue and the risk of infection transmission from the donor to the recipient. Stimulation of the synthesis of extracellular matrix can be achieved very effectively by supplementing keratocyte cultures with vitamin C. The stimulation of human keratocytes to secrete collagen-containing extracellular matrix induced by vitamin C or vitamin C derivatives leads to cell sheets with high cell density. These constructs resemble the matrix that occurs in vivo during corneal development and are therefore considered promising approaches for the in vitro generation of stromal tissue. In initial experiments, we have already been able to show that a material thickness of 100 µm can be generated by cultivating the cell sheets for 12 months, which is relevant for transplantation as a stromal substitute. Furthermore, the stable cell sheets were decellularised, resulting in a cell-free construct with increased biocompatibility. These cell sheets were analysed for their material properties, suturability and their properties as a growth substrate for cells.
Subsequently, the properties of the generated cell sheets in an animal model and their GMP-compliant, standardised production will be investigated so that these matrices can later be used in patients.
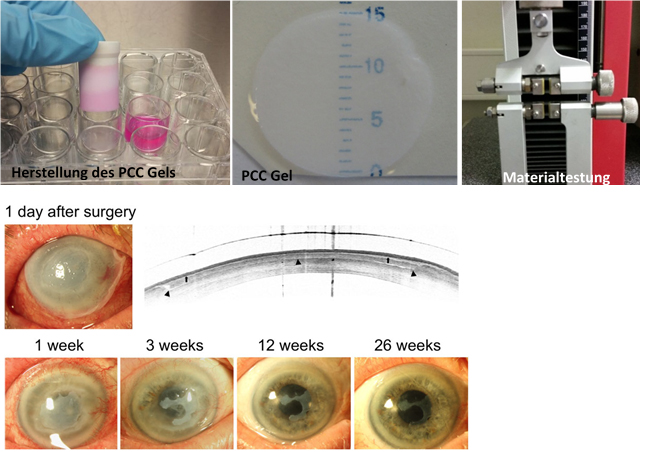
Substance-loaded collagen gels and keratin films
Due to the poor donor rate for corneas to date and the problem of possible rejection reactions etc., there is a great need for the development of new corneal and conjunctival replacement tissues. Among other things, these artificial tissues must be biocompatible, have low quality differences, be suitable as a growth substrate for ocular surface epithelial cells, remain biomechanically stable over a long period of time and be safe for use in humans. Due to these requirements, the search for suitable biomaterials is very difficult, but promising approaches have been described in recent years. In collaboration with the research group of Prof Dr Reichl (Technical University of Braunschweig) and Prof Dr Hansmann (TERM, Würzburg), we have already extensively investigated collagen gels (based on collagen 1) and keratin films (based on hair keratin) as materials for ocular surface reconstruction in vitro and in vivo. Our previous work has shown that keratin-based matrices can be successfully used for corneal surface reconstruction in vitro and in vivo. Furthermore, the successful use of compressed collagen gels as a matrix for conjunctival replacement has been demonstrated in vitro and in vivo.
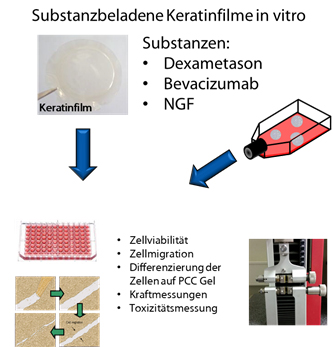
The aim of this project is to further improve these constructs for corneal and conjunctival replacement in order to target specific clinical problems in ocular surface reconstruction. To achieve this, the effects of incorporating different drugs (such as dexamethasone, NGF and bevacizumab) into the two matrices will be investigated in vitro and in vivo.